Therapeutic applications of psilocybin
For decades, research with psychedelics like psilocybin was relegated to the background and hindered by prohibitionist policies that ignored their therapeutic potential. However, this paradigm has changed, and in recent years we have witnessed an unprecedented scientific renaissance, in which this natural compound (present in certain species of fungi of the genus Psilocybe) has returned to the focus of biomedical research.
Unlike the speculative enthusiasm of the 60s, current interest in psilocybin is supported by rigorous clinical trials*, approved by ethics committees and conducted by top-tier academic centers. Institutions such as Johns Hopkins University, Imperial College London, or the University of California San Francisco are leading a new stage in psychiatry, exploring the use of psychedelics not as recreational drugs, but as clinical tools for deep intervention.
This renewed approach does not seek to replace conventional treatments, but to complement them in cases where they have failed: treatment-resistant depression, existential anxiety, substance use disorders, or severe psychological trauma. In this article, we explore the most promising therapeutic applications of psilocybin, based exclusively on published and peer-reviewed scientific evidence.
How does psilocybin act in the brain?
Psilocybin is a prodrug: after being ingested, the organism converts it into its active form, psilocin, which is structurally similar to the neurotransmitter serotonin (5-HT). This similarity allows it to bind to various serotonergic receptors, although its main therapeutic action appears to be mediated by partial agonism of the 5-HT2A receptor, especially in cortical regions.
One of the most studied effects of this interaction is the functional alteration of the Default Mode Network (Default Mode Network, DMN), a brain network associated with self-reference, rumination, and internal narrative. In people with depression or obsessive disorders, this network is usually hyperconnected or overactivated, which contributes to rigid patterns of negative thinking.
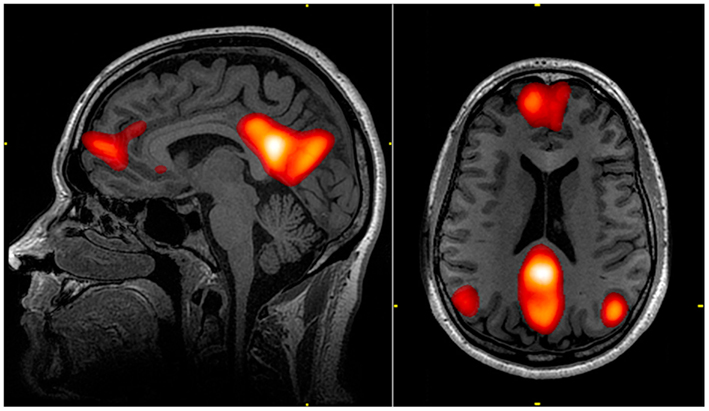
During the psychedelic experience, a temporary disintegration of this network has been observed, along with increased communication between brain regions that normally do not interact with each other. This phenomenon, described as a state of transitory hyperconnectivity, favors the emergence of new cognitive and emotional perspectives. At a therapeutic level, this translates into a kind of neuronal "reset" that can open a window of psychological plasticity, in which patients are more receptive to integrating profound changes through psychotherapy.
This reorganization is not only visible in the electrical and functional activity of the brain, but also in long-term changes in the perception of self, the personal meaning of memories, or the ability to experience emotions with greater intensity and flexibility.
In summary, the therapeutic value of psilocybin does not reside solely in its acute effects, but in its ability to temporarily dissolve entrenched mental patterns and facilitate lasting emotional restructuring, especially when administered in a clinical setting and with psychotherapeutic accompaniment.
Clinical applications with the strongest evidence
Clinical research on psilocybin has advanced rapidly in the last decade, focusing attention on mental disorders that affect millions of people and that, in many cases, do not respond to conventional treatments. Below, we present the three therapeutic areas with the strongest empirical support to date.
Treatment-resistant depression (TRD) and major depressive disorder (MDD)
Treatment-resistant depression represents one of the greatest challenges in contemporary psychiatry. It is estimated that up to one-third of patients with depression do not improve significantly with current antidepressants. In this context, psilocybin has emerged as a potentially transformative alternative.
Clinical studies conducted at Johns Hopkins University and Imperial College London have demonstrated that one or two psilocybin sessions, accompanied by structured therapeutic support, can induce rapid and sustained improvements in depressive symptoms. A 2020 trial published in JAMA Psychiatry [1] showed that participants with major depressive disorder presented significant improvements in their mood and emotional functioning just one week after administration, with effects that were maintained for at least four weeks.
Additionally, a multicenter phase 2b clinical trial led by COMPASS Pathways [2] , and published in the New England Journal of Medicine in 2022, found that a single dose of 25 mg of synthetic psilocybin significantly reduced symptoms of treatment-resistant depression, with benefits that persisted for several months in many patients. In some secondary criteria, psilocybin's efficacy was comparable or superior to that of conventional antidepressants, without requiring daily doses or generating dependence.
These results suggest that psilocybin could reconfigure the way we treat depression, not as a chronic process to be controlled indefinitely, but as a transformative experience facilitated by neuroplasticity and therapeutic accompaniment.
Anxiety and depression in patients with terminal illnesses
Another of the most consolidated applications of psilocybin is the treatment of psychological distress in people with serious or terminal illnesses, such as advanced cancer. In these cases, emotional suffering usually includes existential anxiety, fear of death, hopelessness, and isolation, states that traditional pharmacological treatments rarely alleviate effectively.
Clinical studies developed by research teams at Johns Hopkins University and New York University [3] demonstrated that a single dose of psilocybin, administered in a clinical setting and with therapeutic accompaniment, can rapidly and lastingly reduce symptoms of anxiety and depression in cancer patients. In long-term follow-up, more than 80% of participants reported significant improvements in their emotional well-being, perception of meaning, and acceptance of their own mortality.
This effect is not explained solely by brain chemistry, but also by the profoundly meaningful quality of the psychedelic experience, which many patients describe as one of the most important of their lives. This existential dimension, which transcends clinical symptoms, is one of the aspects that differentiates psilocybin-assisted therapy from conventional approaches.
Substance use disorders (addictions)
Psilocybin is also being studied as a therapeutic tool to address substance use disorders, including tobacco, alcohol, and other drug dependencies. Unlike traditional treatments, which usually focus on symptom suppression or behavioral control, the psychedelic experience facilitates a deep review of thought patterns, motivation, and self-perception, which can be especially useful in rehabilitation processes.
A pioneering 2014 study conducted by the Johns Hopkins University team [4] showed that two or three psilocybin sessions combined with cognitive-behavioral therapy helped 80% of participants quit smoking, remaining abstinent for at least six months, a rate much higher than that obtained with standard treatments.
Similar results have been observed in alcoholism treatment. A trial published in 2022 in JAMA Psychiatry [5] revealed that two doses of psilocybin, administered within a psychotherapeutic program, reduced excessive alcohol consumption by 83% during follow-up. Participants also reported improvements in emotional control, sense of purpose, and quality of life.
These findings suggest that psilocybin does not act only on addiction symptoms, but on the psychological and existential factors that sustain it, opening new treatment avenues in one of the most difficult areas of mental health.
Emerging applications in research
Beyond its applications in depression, existential anxiety, and addictions, psilocybin is being studied in other complex psychiatric conditions. Although the results are still preliminary, several ongoing trials are yielding promising indications about its possible efficacy in disorders such as OCD, post-traumatic stress, or certain neurological conditions. Below are some of the most relevant lines of research.
Obsessive-compulsive disorder (OCD)
Obsessive-compulsive disorder (OCD) is characterized by recurrent intrusive thoughts and compulsive behaviors designed to reduce anxiety. Although effective treatments exist, such as serotonin reuptake inhibitors (SSRIs) and cognitive-behavioral therapy, a considerable proportion of patients do not respond adequately.
Psilocybin is being investigated as a possible alternative to interrupt obsessive-compulsive cycles, acting on the hyperactivity of certain brain networks associated with self-reference and control. In a pilot study conducted by Francisco Moreno and collaborators (2006) [6], an acute reduction of OCD symptoms was observed in patients who received psilocybin in variable doses. Although the sample size was small and the design was not double-blind, the results opened a line of research that continues to expand.
New, more robust clinical trials are currently being developed to determine if these effects can be replicated consistently and sustainably.
Post-traumatic stress disorder (PTSD)
Post-traumatic stress disorder (PTSD) involves a profound alteration in memory, emotional regulation, and perception of the world following a traumatic experience. Although the most advanced approach in this field has been the use of MDMA-assisted psychotherapy, psilocybin is beginning to be studied as a tool that could facilitate the restructuring of traumatic memories in a safe clinical environment.
Ongoing studies explore the hypothesis that the psychedelic experience could allow the patient to reconnect with painful events from a less reactive and more integrative emotional state, promoting processes of re-signification and emotional liberation. Although the results are not yet conclusive, it is considered a promising line in combination with trauma-specialized psychotherapy.
Bipolar depression
Traditionally, patients with bipolar disorder, especially type I, have been excluded from clinical trials with psychedelics due to the risk of inducing manic or psychotic episodes. However, recent research is beginning to carefully explore the safety and efficacy of psilocybin in people with bipolar type II disorder, characterized by major depressive episodes without full mania.
A preliminary, non-randomized study evaluated the safety of psilocybin in patients with bipolar type II under controlled psychedelic therapy conditions [7]. The results, although limited by the small sample size, suggested that supervised administration of psilocybin did not trigger manic or psychotic symptoms, and that it could have sustained antidepressant effects in some cases.
These findings suggest that, with rigorous patient selection, absence of mania history, and intensive psychotherapeutic accompaniment, psilocybin could represent a therapeutic avenue for treatment-resistant bipolar depression. However, this line of research is still in very early stages and requires randomized studies, with larger samples and long-term follow-up, before being considered clinically viable.
Chronic pain and fibromyalgia
Another emerging research area focuses on the treatment of chronic pain, especially in conditions with a strong psycho-emotional component, such as fibromyalgia. Unlike conventional analgesics, psilocybin does not act directly on nociceptors, but modulates pain perception through changes in consciousness, emotionality, and the patient's relationship with their suffering. In this context, psilocybin could reduce the affective component of pain by facilitating states of acceptance and recontextualization.
Pilot studies have shown that patients with fibromyalgia experienced greater pain tolerance, better functionality, and reduction of depressive symptoms after psilocybin sessions. For example, a registered clinical trial [8], currently ongoing, specifically explores the safety and efficacy of psilocybin in patients with fibromyalgia.
Similarly, the University of California San Francisco (UCSF) is developing a phase 1/2 trial to evaluate the efficacy of this substance in chronic low back pain management, with attention to both pain reduction and treatment of comorbid symptoms such as anxiety, hopelessness, or fatigue. While initial results are promising, it is essential to emphasize that psilocybin should not be considered an analgesic, but a psychotherapeutic intervention that addresses pain from an integrative perspective, acting on both body and mind.
Other lines of clinical research with psilocybin
Various investigations are also exploring the use of psilocybin in social anxiety disorders, especially in people with autism spectrum disorders, as well as in eating disorders such as anorexia nervosa, where cognitive rigidity and emotional control play a key role.
Additionally, some pilot studies have observed beneficial effects of psilocybin in chronic migraines [9] and cluster headaches [10] , possibly due to its action on cerebral vasculature and modulation of the serotonergic system.
Although these applications are in an early stage of development, they represent a fertile field for future research, especially if clinical results continue to show a favorable profile of safety and efficacy.
While these results are encouraging, enthusiasm must be tempered by deep consideration of the ethical, legal, and safety challenges that still surround psilocybin.

Ethical, legal, and clinical considerations
Despite growing enthusiasm around psilocybin's therapeutic potential, its clinical application continues to be surrounded by fundamental precautions. Both researchers and professionals agree that it is not a "magic cure," but a powerful tool that can only unleash its full value when administered under strictly controlled conditions. Ignoring this context can not only reduce its efficacy but put the patient's psychological health at risk.
Safety and contraindications
Although psilocybin has shown a favorable safety profile in clinical studies, it is not exempt from risks, especially when used without adequate accompaniment. Among the most common side effects are acute anxiety, confusion, nausea, or emotional discomfort during the experience.
In clinical contexts, these effects are usually transitory and manageable, but in people with previous psychiatric vulnerability, such as personal or family history of psychosis or bipolar disorder, the use of psilocybin can trigger serious adverse effects.
Therefore, prior medical and psychological evaluation is an essential requirement for any therapeutic protocol with psilocybin. Additionally, its use is excluded in minors, pregnant women, and in combination with certain medications, such as monoamine oxidase inhibitors (MAOIs) or antipsychotics.
Legal status of psilocybin and current access (August 2025)
Despite the scientific boom, psilocybin remains a controlled substance in most countries, where it is classified as a prohibited drug without recognized therapeutic value. However, this status is beginning to change thanks to pressure from the scientific and medical community.
- In the United States, the state of Oregon legalized therapeutic use of psilocybin under professional supervision in 2020, and Colorado approved a similar measure in 2022.
- In Australia, starting in 2023, authorized psychiatrists can prescribe psilocybin for treatment-resistant depression.
- In Switzerland, certain psilocybin treatments are possible under compassionate use protocols and with specific authorization.
- The European Medicines Agency (EMA) and other regulatory entities are already receiving data from ongoing clinical trials that could lead to future conditional approval on the continent.
Meanwhile, legal access is limited to approved clinical trials, compassionate use programs, and accredited research centers. Any use outside this framework remains illegal in most jurisdictions and carries both personal and legal risks.
The renaissance of interest in psilocybin is not a fad or nostalgia for the sixties, but the result of more than two decades of rigorous scientific research. The accumulation of clinical data on its efficacy in disorders such as treatment-resistant depression, existential anxiety, or addictions raises a profound revision of the current biomedical model, which has often offered partial answers to problems of emotional and existential origin.
However, it is not advisable to fall into triumphalism. Psilocybin is not a panacea and its therapeutic application cannot be separated from the context in which it is administered: it requires precise clinical protocols, qualified professional accompaniment, and an integration process that allows translating what was experienced into meaningful changes. Its efficacy is closely linked to factors such as intention, environment, and the therapeutic bond, which cannot be replicated outside the clinical setting.
As phase III clinical trials are completed and regulatory frameworks begin to adapt, we are approaching a new stage: that of psychedelic-assisted psychiatry, focused on subjective experience, neuroplasticity, and the potential for personal transformation. In this emerging scenario, psilocybin not only represents a promising drug, but also a paradigm shift in our way of understanding and treating psychic suffering.
The challenge now is twofold: to guarantee ethical and safe access to these therapies for those who need them, and to avoid their trivialization or premature commercialization, which could compromise decades of scientific and social progress. Only through prudence, evidence, and active listening can we integrate this ancestral knowledge into the medicine of the future.
References
- Davis, A. K Barrett et al. (2020). Effects of Psilocybin‑Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry, 78 (5): 481–489. DOI: 10.1001/jamapsychiatry.2020.3285
- Carhart-Harris RL, et al. (2021). NEJM, 384 (15), 1402-1411. DOI: 10.1056/NEJMoa2032994
- Griffiths RR, Davis, A. K.; Barrett (2016). J Psychopharmacol, 30 (12), 1181-1197.
Ross S, et al. (2016). J Psychopharmacol, 30 (12), 1165-1180.
DOI: 10.1177/0269881116675513 - Johnson MW, et al. (2014). J Psychopharmacol, 28 (11), 983–992. DOI: 10.1177/0269881114548296
- Bogenschutz MP, et al. (2022). JAMA Psychiatry, 79 (10), 953–962. DOI: 10.1001/jamapsychiatry.2022.2096
- Moreno FA, et al. (2006). J Clin Psychiatry, 67 (11), 1735–1740. DOI: 10.4088/JCP.v67n1110
- Scott T. Aaronson et al. (2024). Single-Dose Synthetic Psilocybin With Psychotherapy for Treatment-Resistant Bipolar Type II Major Depressive Episode. JAMA Psychiatry, 81(6), 555-562. DOI: 10.1001/jamapsychiatry.2023.4685
- University of Alabama at Birmingham (2025). Psilocybin for the Treatment of Fibromyalgia (NCT05068791)
- Sexton, L. J., & Misra, S. K. (2021). Safety and efficacy of psilocybin in the treatment of chronic migraines. Journal of Clinical Medicine, 10(10), 2148. DOI: 10.3390/jcm10102148
- Rebar, C., et al. (2024). Effects of Psilocybin on Cluster Headache: A Systematic Review. Journal of Clinical Pharmacology and Therapeutics. DOI: 10.1111/jcpt.14081




















